What is Healthcare Value Management?
Health care Value Management is an approach to health care delivery. It emphasizes maximizing value by achieving the best health outcomes at the lowest cost based on a patient’s condition. This approach was defined by healthcare SMEs and supported by leading healthcare organizations around the world
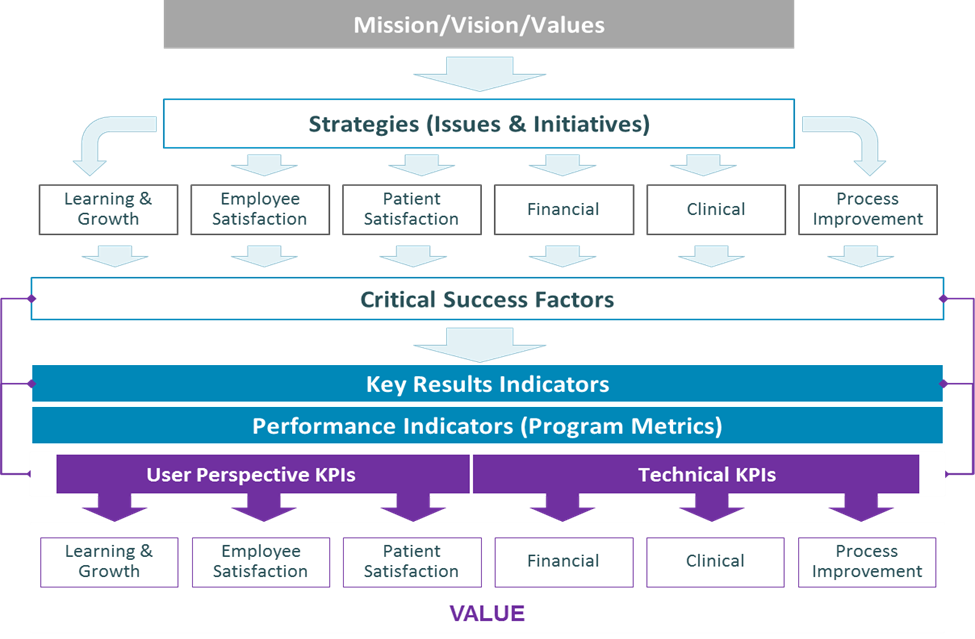
What is the Value Realization Framework?
What are the six perspectives in the Value Realization Framework?
There are six measurable perspectives to Healthcare Value Management. They are a combination of process and stakeholder perspectives of a business that are encapsulated in the Value Scorecard, which is comprised of six perspectives:
Financial – Increased revenue by leveraging data to quickly negotiate with payers (i.e. private insurance/Medicare)
Clinical – Improved clinical data-driven decision-making to deliver high quality and safe patient-centered care
Process Improvement – Decreased clinical, administrative, and other resource costs (e.g. elimination of paper/material costs) and improve efficiencies
Learning and Growth – Increased expertise and adaptability by capturing lessons learned and improving best practices
Patient Satisfaction – Measured value of patient satisfaction and experience
Employee Satisfaction – Measured value and patient experience, which leads to improved recruiting, retraining, and retaining of employees
What are the key concepts that constitute the core of Value Management include the following terms:
- Outcomes – A measure of results and benefits from strategic initiatives across six perspectives in healthcare, such as Patient and Employee Satisfaction, Clinical and Financial Outcomes, Process Improvement and Learning, and Growth.
- Critical Success Factors (CSFs) – “The key areas where an organization must perform well on a consistent basis to achieve its mission.”[i]
- Key Results Indicators (KRIs) – A “measure of the results from your business actions which are critical in tracking progress and defining success.”
- Performance Indicators (PIs) – A “particular characteristic or dimension used to measure intended changes defined by an organizational unit’s results framework. Performance indicators are used to observe progress and to measure actual results compared to expected results. They serve to answer “how” or “whether” a unit is progressing towards its objectives, rather than “why” or “why not” such progress is being made. Performance indicators are usually expressed in quantifiable terms, and should be objective and measurable (e.g., numeric values, percentages, scores, and indices).”
- Key Performance Indicators (KPIs) – A “measure of the actions and events that lead to a result and are considered to be critical to the success of your business as their data is crucial in creating strategies and aligning goals.”
- User Perspective KPIs – System performance that impacts Usability and Customer Satisfaction based on availability, efficiency, and the accuracy of the systems.
- Technical KPIs – System performance that impacts managing the collective enterprise architecture and network functionality of systems.
- Value Elements – A quantifiable, calculated benefit that is worth the investment.
It is critical that effectiveness is defined first i.e. desired outcomes prior to planning for efficiency, otherwise, there is risk of doing the wrong things well.
Sources: Carnegie Mellon definition of Critical Success Factors, 2015; Parmenter, David. Key Performance Indicators (KPI): Developing, Implementing, and Using Winning KPIs. 2007; Handbook on Monitoring and Evaluating for Results. United Nations Development Programme, Evaluation Office, NY, 2002.
[i] Carnegie Mellon definition of Critical Success Factors, 2015
How do outcomes shape the future delivery of healthcare?Consolidation Loans be deferred?
Outcomes empower patients, providers, and payers and will influence the future healthcare delivery landscape in three distinct ways:
1. Patients shall choose the providers for their care based on outcome value scores
2. Providers shall be data-informed to make targeted improvements and learn
3. Payers shall measure return on investment and direct patients to high-value providers
